HCG Trigger Timing Calculator
Calculate Your IVF Window
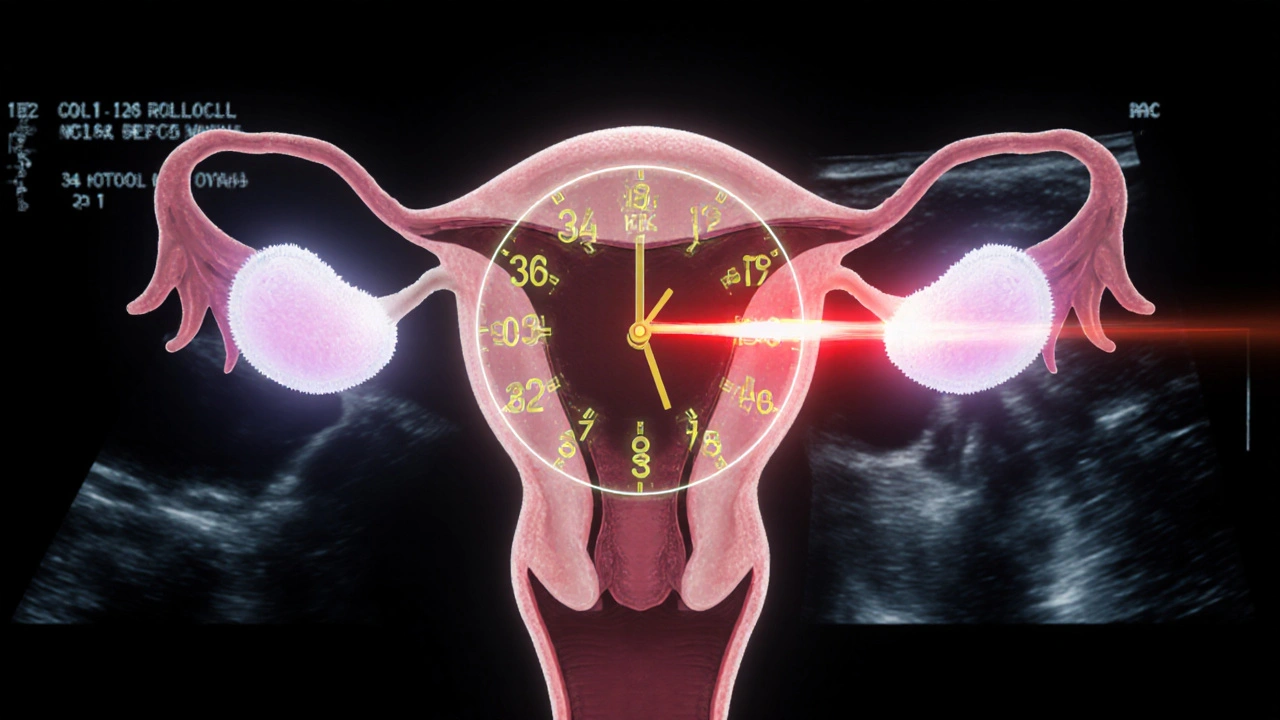
Determine your precise egg retrieval window based on your HCG trigger shot timing. The 34-36 hour window is critical for maximizing mature egg yield.
Enter your trigger shot time to see your optimal retrieval window.
When you’re going through IVF, one of the most nerve-wracking moments isn’t the egg retrieval itself - it’s the HCG trigger shot. Get the timing wrong by even an hour, and you could lose half your mature eggs. This isn’t theory. It’s what happens in real clinics, every day.
Why the HCG Trigger Shot Matters
The HCG trigger shot isn’t just another injection. It’s the final command that tells your body: release the eggs now. In a natural cycle, your body produces a surge of luteinizing hormone (LH) to trigger ovulation. But in IVF, you’re on medications that suppress your natural cycle. So doctors use synthetic HCG - a hormone that acts just like LH - to mimic that surge on their schedule. Without this shot, eggs won’t mature properly. But if you give it too early or too late, you risk premature ovulation. That means the eggs are released into your fallopian tubes before the clinic can retrieve them. And once they’re gone, they’re gone. No second chances.The 34- to 36-Hour Window
Every clinic gives you a specific time to take your trigger shot - often down to the minute. Why? Because eggs need exactly 34 to 36 hours to complete their final maturation after HCG is injected. That’s not a guess. It’s biology. During those 36 hours, the egg goes through a critical change: it reduces its chromosomes from 46 to 23. This is called meiosis II. If the egg isn’t retrieved within that window, it either matures too late (and becomes non-viable) or it’s already released. Studies show that a delay of just 12 hours can drop your mature egg count by 15-20%. A 90-minute delay? Up to 25% loss. That’s why patients set three alarms. Why some people sleep with their injection kit beside them. Why Reddit threads are full of stories like: “I gave my shot at 10 PM instead of 8 PM - lost 7 of 12 eggs.”Types of HCG Triggers
Not all trigger shots are the same. The two main types are:- Pregnyl: 10,000 IU of hCG, given as an intramuscular injection. Used in about 60% of U.S. clinics.
- Ovidrel: 250 mcg of recombinant hCG, given as a subcutaneous injection. Less painful, easier to self-administer. Used in 40% of cases.
When Do You Get the Shot?
Your doctor won’t give you the trigger shot just because you’ve been on stimulation for 10 days. They wait for signs that your follicles are ready:- At least three follicles are 17-20 mm in size (measured by ultrasound)
- Your estradiol level is above 200 pg/mL per mature follicle
- Your progesterone is still low (high levels mean ovulation is already starting)
What Happens If You’re Late?
Let’s say your clinic told you to take the shot at 8:00 PM. You’re tired. You forget. You take it at 10:00 PM. What happens? You might not notice anything right away. But when you get to the clinic for retrieval, they’ll find fewer mature eggs. Maybe half of them are overripe. Some may have already ovulated. Your fertilization rate drops. Your chance of pregnancy drops too. One 2022 study tracked 342 IVF cycles where patients missed their trigger window. Of those, 41% had 25% fewer mature eggs. And 12% had zero retrievable eggs. That’s not a small risk. That’s a cycle-ending mistake. Patients who use reminder apps, phone alarms, or even a “trigger buddy” (a nurse who calls 30 minutes before) have near-zero errors. Clinics that give detailed, written instructions - not just a verbal reminder - see 60% fewer timing mistakes.Who Should Avoid HCG?
HCG is powerful. But it’s not for everyone. If you’re at high risk for OHSS - which happens when your ovaries become dangerously swollen - HCG can make it worse. Signs you’re at risk:- High AMH levels (over 4 ng/mL)
- Polycystic ovary syndrome (PCOS)
- More than 20 mature follicles
- Previous OHSS

What’s New in Trigger Timing?
The field is moving beyond just follicle size and hormone levels. In 2023, researchers at UC San Francisco launched an AI tool that analyzes ultrasound images and hormone trends to predict the exact moment to trigger - within a 90-minute window. Early results show 85% accuracy. Other clinics are using anti-Müllerian hormone (AMH) levels to fine-tune timing. If your AMH is high, they trigger earlier. If it’s low, they wait longer. This personalization is cutting premature ovulation rates from 8.7% to 6.8%. Still, not everyone agrees. Some doctors worry we’re overcomplicating things. “The pursuit of perfect timing,” says Dr. Richard Grazi, “is creating panic for patients when the real risk is smaller than we make it seem.”How to Prepare for Your Trigger Shot
If you’re about to take your HCG trigger, here’s what actually works:- Get written instructions - not just a text message. Ask for a one-page checklist.
- Set three alarms - one for 30 minutes before, one for the exact time, one for 10 minutes after.
- Keep your kit ready - pre-filled syringe, alcohol wipes, bandage. Store it in the fridge until use.
- Practice the injection - most people learn in 20 minutes with a nurse. Don’t wing it.
- Have someone with you - even if it’s just a text chain with a friend who says, “Are you ready?”
Final Thought: Precision Isn’t Perfection
Yes, timing matters. But perfection isn’t the goal. Consistency is. Most clinics report that even patients who are 1-2 hours off still have successful cycles - as long as they’re not 4 hours late. The real win? Knowing the science behind it. Understanding why you’re doing this. And trusting your team. Because the trigger shot isn’t just about biology. It’s about control. In a process full of uncertainty, this is one thing you can get right.What happens if I miss my HCG trigger shot by an hour?
Missing your trigger shot by an hour usually doesn’t ruin the cycle. Most clinics allow a 30-60 minute window. But delays beyond 90 minutes can reduce mature egg yield by up to 25%. If you’re late, call your clinic immediately - they may adjust retrieval timing or give you a rescue dose.
Is Ovidrel better than Pregnyl?
Both are equally effective at triggering ovulation. Ovidrel is subcutaneous (less painful, easier to self-administer) and preferred by most patients. Pregnyl is intramuscular and slightly cheaper. The choice often comes down to patient comfort and clinic protocol - not effectiveness.
Can I take the HCG trigger shot at home?
Yes, most patients administer the trigger shot at home. Your clinic will train you on how to inject it properly - whether it’s subcutaneous (Ovidrel) or intramuscular (Pregnyl). You’ll get step-by-step instructions, and many clinics offer follow-up calls to confirm you did it right.
Why do I need to refrigerate my HCG trigger?
HCG is a protein-based hormone that breaks down at room temperature. Unreconstituted vials must be stored at 36-46°F (2-8°C) until mixed. Once mixed, it’s stable for 24-48 hours at room temperature. Always check the manufacturer’s instructions - some brands have different rules.
Are there alternatives to HCG for triggering ovulation?
Yes. GnRH agonists like Lupron can trigger ovulation without the OHSS risk. They’re often used for high-risk patients. But they typically yield fewer eggs. A dual trigger - combining a small dose of HCG with Lupron - is becoming popular because it balances egg yield and safety.
How do I know if my trigger shot worked?
You won’t feel it. The only way to know is through egg retrieval. If you have a high number of mature eggs retrieved (usually 8-15), the trigger worked. If you have very few or none, it may have been too early or too late. Your clinic will analyze egg maturity under the microscope after retrieval.
Can I take the HCG trigger shot during the day instead of at night?
Yes - if your clinic schedules retrieval for the afternoon, they’ll give you a daytime trigger time. Many clinics now schedule retrieval between 11 AM and 2 PM, so the trigger is given around 7-9 AM. Night triggers are only needed if retrieval is early morning. Always follow your clinic’s specific timing.