Birth Control Pill Effectiveness Calculator
Estimated Pregnancy Rate
--
Pregnancies per 100 women per year
Key Factors: Your risk depends on:
- Whether you take it perfectly
- How often you miss doses
- Which pill type you're using
Note: The Pearl Index is the number of pregnancies per 100 women per year. For example, a rate of 2.74 means 2.74 pregnancies would occur among 100 women using this method for a year.
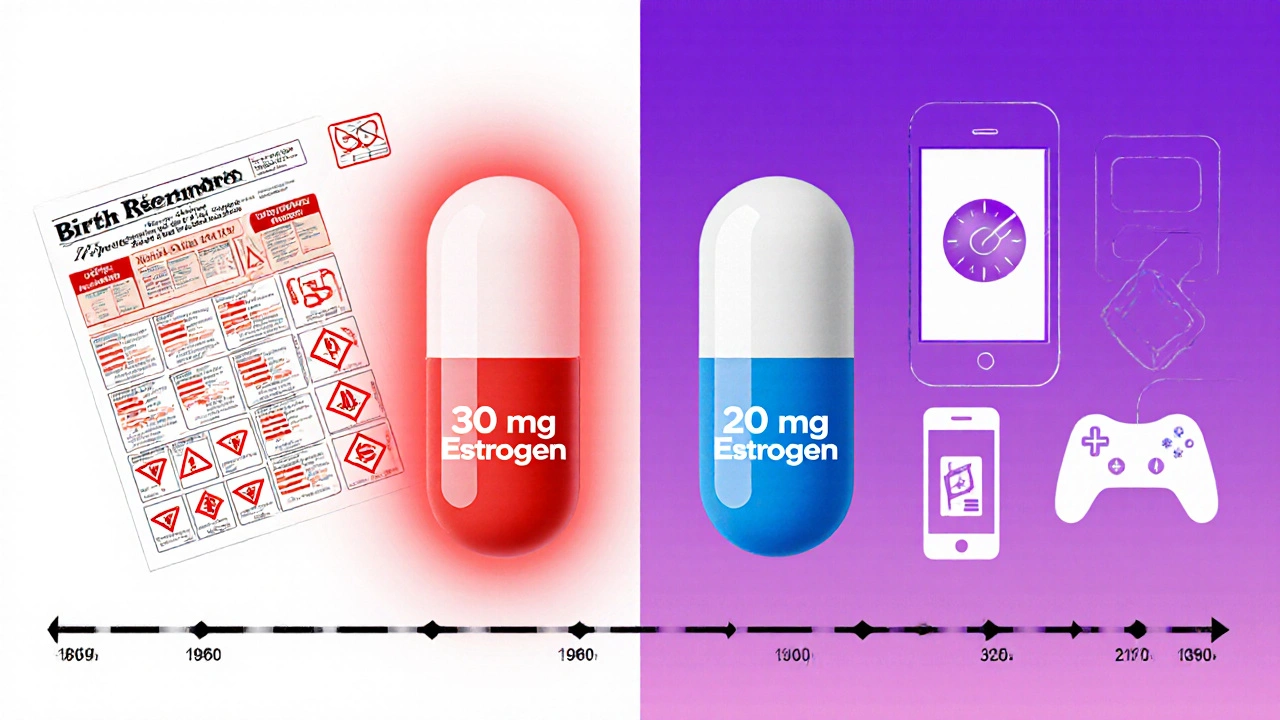
When birth control pills first hit the market in 1960, they packed a punch-up to 175 micrograms of estrogen. Women took them to prevent pregnancy, but many also dealt with nausea, weight gain, headaches, and sometimes serious blood clots. Today’s pills are different. Most contain less than half the estrogen of even the low-dose pills from the 1990s. The question isn’t just whether they still work-it’s whether they work well enough without the side effects that made earlier versions hard to tolerate.
How Low Is Too Low? The Hormone Numbers That Matter
Modern birth control pills come in two main types: combined (estrogen + progestin) and progestin-only. The estrogen in most combined pills today is ethinyl estradiol (EE), and doses range from 10 to 35 micrograms. The standard "low-dose" label applies to pills with 20-35 mcg EE. Pills with 10-20 mcg EE are called "ultra-low-dose." That’s a 70% drop from the original 1960s formula.Progestin-only pills (POPs), sometimes called the "mini-pill," contain no estrogen at all. Common versions include norethindrone (0.35 mg), norgestrel (0.075 mg), and drospirenone (4 mg). These are often prescribed for women who can’t take estrogen due to migraines with aura, high blood pressure, or a history of blood clots.
Here’s the key: lowering hormones doesn’t mean lowering effectiveness-if you take them right. A 2010 study tracking over 1,200 women found that the ultra-low-dose pill (EE 20 mcg + LNG 100 mcg) had a Pearl Index of 2.74 (meaning 2.74 pregnancies per 100 women per year). Compare that to the older EE 30 mcg + LNG 150 mcg pill, which had a Pearl Index of 0.60. At first glance, that seems like a big difference. But here’s the catch: the 2.74 figure includes women who missed pills. Among those who took it perfectly, the rate dropped to 1.73. That’s still close to the 0.60 of the higher-dose pill. The difference isn’t in the pill-it’s in the user.
Effectiveness: It’s Not the Dose, It’s the Timing
All hormonal birth control pills are less effective in real life than in clinical trials. Why? Because people forget. Or take them late. Or throw them out because of spotting.The CDC reports that with perfect use, all combined hormonal methods (pills, patches, rings) result in about 2 pregnancies per 100 women per year. With typical use? That jumps to 4-7. That’s the same for high-dose and low-dose pills. The hormone level doesn’t change how often people miss doses-it’s the behavior.
Progestin-only pills are even more timing-sensitive. You have to take them within a 3-hour window every day. Miss that window, and ovulation can happen. A 2022 JAMA study found that when women took their drospirenone pill 24 hours late, one out of 127 showed signs of ovulation. That’s rare-but it’s enough to worry about. Higher-dose combined pills give you a little more wiggle room-up to 12-24 hours. That’s why some women switch to low-dose pills and then panic when they start spotting or get pregnant. It’s not the pill failing. It’s the routine breaking.
Safety: Are Lower Hormones Safer?
The original high-dose pills carried a clear risk: blood clots, strokes, and heart attacks. That’s why doctors started lowering estrogen in the 1980s. Today, the risk is tiny-but not zero.For a healthy woman under 35 with no risk factors, the chance of a blood clot from a low-dose pill is about 5-10 per 10,000 women per year. That’s lower than the risk during pregnancy (about 29 per 10,000). The American Heart Association confirms that modern low-dose pills (10-35 mcg EE) have reduced this risk significantly compared to older versions.
But here’s the twist: lowering estrogen from 30 mcg to 20 mcg doesn’t lower that risk any further. Dr. Sarah Prager from the University of Washington says there’s no clinical evidence that 20 mcg is safer than 30 mcg when it comes to clots. The same goes for progestin doses. Dr. Marc LaPointe pointed out in 2021 that no study has shown a benefit to lowering levonorgestrel from 150 mcg to 100 mcg. So why do manufacturers make ultra-low-dose pills? Because women want them. Because they feel better.
Side Effects: Less Nausea, More Spotting
The biggest win with low-hormone pills? Fewer estrogen-related side effects. A 2023 Reddit analysis of over 1,200 posts found that 38% of women who switched from 30 mcg to 20 mcg EE reported their nausea disappeared. Another 29% said their periods became lighter or stopped altogether.But there’s a trade-off. Breakthrough bleeding-spotting between periods-is the #1 complaint. A review of 8,432 Healthline reviews showed 42% of negative feedback centered on spotting. One woman on WebMD wrote: "Since switching to the 20 mcg pill, I’ve had spotting almost daily and worry it’s not working as well."
That spotting is usually harmless. ACOG says 30-40% of users experience it in the first 3-6 months, and it almost always fades. But it’s enough to make people quit. A 2023 Guttmacher survey found that 37% of women under 21 stopped using low-dose pills within a year, compared to 29% of older women. For teens, spotting feels like failure. They don’t know it’s normal.
Who Should Use Low-Hormone Pills?
Low-hormone pills are ideal for:- Women who had bad side effects from higher-dose pills (nausea, breast tenderness, headaches)
- Those with estrogen contraindications (migraines with aura, history of clots, high blood pressure)
- People who want lighter periods or no periods at all
- Women who can take a pill at the same time every day
They’re not ideal for:
- Women who frequently forget pills or take them late
- Teens who are still building routines
- Anyone who can’t handle spotting
For those who struggle with timing, long-acting methods like IUDs or implants are far more effective. A 2022 study of 10,000 U.S. users found that LARCs had a pregnancy rate of 0.27 per 100 women per year-compared to 4.55 for pills. That’s a 17-fold difference.

What’s New in 2025?
The biggest change? Opill, the first progestin-only pill approved for over-the-counter sale in the U.S. in April 2024. It contains norgestrel (0.075 mg) and has a typical-use Pearl Index of 3.4. That’s higher than prescription POPs, but still effective if taken correctly. It’s a game-changer for access-no prescription needed.Researchers are already working on next-gen pills. A February 2025 study in Nature Communications is testing new progestins that suppress ovulation at even lower doses. Early Phase 2 trials show promise with 10 mcg EE formulations. By 2028, McKinsey predicts 75% of new birth control pills will contain 25 mcg EE or less.
Meanwhile, the market is shifting. In 2023, 58% of all birth control pills prescribed in the U.S. were low-dose (20-30 mcg EE), up from 42% in 2018. Extended-cycle pills (taking active pills for 84 days straight) are also growing in popularity, with 22% of OB/GYNs reporting increased prescriptions in the last two years.
How to Make It Work
If you’re on a low-hormone pill, here’s how to avoid failure:- Set a daily phone alarm-even if you’re on a combined pill, set it for the same time every day.
- Use an app like MyPill or Birth Control Reminder. A 2024 study found users had 23% fewer missed doses.
- For progestin-only pills: never go more than 3 hours late. If you do, use backup contraception (condoms) for 48 hours.
- Don’t panic about spotting. It’s normal. Wait 3-6 months before switching.
- Keep a spare pack. Run out? Call your pharmacy. Most have 24/7 refill services.
And if you’re still unsure? Talk to your provider. There’s no one-size-fits-all pill. What works for your friend might not work for you. The goal isn’t the lowest dose-it’s the dose that keeps you safe, comfortable, and pregnancy-free.
Frequently Asked Questions
Are low-hormone birth control pills less effective than older ones?
No, not if taken correctly. Studies show ultra-low-dose pills (10-20 mcg estrogen) have pregnancy rates nearly identical to higher-dose pills when used perfectly. The difference isn’t in the hormone level-it’s in how consistently people take them. Missed pills are the main cause of failure, not low doses.
Why am I spotting all the time on my low-dose pill?
Spotting is very common in the first 3-6 months, especially with low-hormone pills. Your body is adjusting to less estrogen. It doesn’t mean the pill isn’t working. Most women stop spotting after a few cycles. If it continues past six months or becomes heavy, talk to your provider about switching progestins.
Can I switch from a 30 mcg pill to a 20 mcg pill safely?
Yes. Many women switch to reduce nausea or breast tenderness. Start the new pill on the same day you’d start your next pack. You don’t need a break. Expect some spotting at first-it’s normal. If you had no side effects on the higher dose, there’s no medical reason to switch unless you want to.
Is Opill (the over-the-counter pill) as good as prescription pills?
Opill (norgestrel 0.075 mg) is a progestin-only pill with a typical-use failure rate of 3.4 pregnancies per 100 women per year-slightly higher than prescription POPs, but still effective. It’s not for everyone. You must take it within 3 hours every day. If you forget often, a combined pill or LARC might be better. But for those who can be consistent, it’s a safe, accessible option.
Should I choose a low-hormone pill over an IUD?
If your main concern is effectiveness, an IUD or implant is far better. They’re over 99% effective and last for years without daily effort. Pills are better if you want to control your cycle, avoid surgery, or plan to get pregnant soon. But if you’re someone who forgets to take pills, an IUD is the smarter choice.




