Dalkon Shield vs. Modern IUD Comparison Tool
Design Flaw: Multifilament cotton string with unsealed ends acted as a wick, drawing bacteria into the uterus.
Regulatory Status: Approved under FDA's 'grandfather clause' with no clinical trials required.
Impact Statistics:
• Over 200,000 women developed pelvic inflammatory disease
• 18 confirmed deaths
• Over 100,000 women required hysterectomies
• Nearly 300,000 lawsuits filed
Human Cost: Millions affected with life-altering injuries and permanent fertility loss
Safety Feature: Single-filament strings sealed at both ends to prevent bacterial wicking.
Regulatory Status: Rigorous FDA clinical trials required before market approval (Class III devices).
Current Safety Data:
• PID risk: < 1% with proper insertion
• 99% effective long-term contraception
• Over 10 million women use modern IUDs safely
• 100% of IUDs undergo FDA post-market surveillance
Modern Impact: Safer for millions of women with extensive medical oversight
Based on the Dalkon Shield's 7.5% infection rate (over 3 million users) and modern IUD's <1% infection rate, here's the comparison:
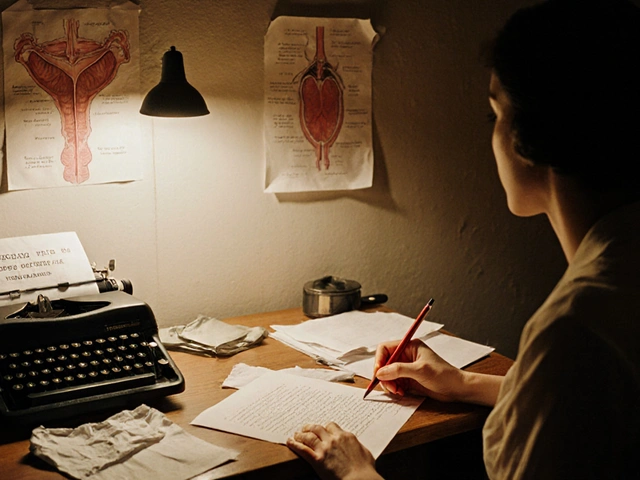
The Dalkon Shield wasn’t just a bad birth control device. It was a betrayal. In the early 1970s, over three million American women trusted it to prevent pregnancy. They didn’t know the string inside it was designed to pull bacteria into their bodies. By the time the truth came out, thousands were injured, dozens were dead, and the system meant to protect them had failed completely.
How a ‘Miracle’ IUD Became a Death Trap
The Dalkon Shield looked like science fiction made real. Invented by a Johns Hopkins gynecologist and an engineer, it had a unique, star-shaped frame that was supposed to hold it securely in place. The company, A.H. Robins, marketed it as 99% effective-better than the pill, which was under fire for blood clots and strokes. It was promoted as the future of contraception: long-lasting, hormone-free, and foolproof. But the real danger wasn’t in the metal or plastic. It was in the string. Unlike other IUDs, the Dalkon Shield used a multifilament string made of cotton fibers wrapped in plastic. The ends weren’t sealed. That meant when a woman inserted it, the string could act like a wick, drawing bacteria from the vagina straight into the uterus. It was a design flaw so obvious, an employee warned the company in 1970. They ignored it. By 1974, the damage was undeniable. Women were getting pelvic inflammatory disease (PID) at alarming rates. Many developed septic abortions. Some lost their fertility. Others died. The FDA had no power to stop it because, under the law at the time, medical devices didn’t need clinical trials. The Dalkon Shield was approved under a loophole called the ‘grandfather clause’-just because older IUDs existed, this one got a pass.The Human Cost Nobody Wanted to See
The numbers are chilling: over 200,000 women developed PID. At least 18 died. More than 100,000 women had to undergo hysterectomies. Many needed lifelong hormone therapy. Some were told they’d never have children again. But the physical damage was only half the story. The legal battles that followed were brutal. Women who sued were grilled about their sex lives in court. Lawyers asked invasive questions. Juries often didn’t believe them. Compensation? Most victims got between $750 and $2,000. Adjusted for inflation, that’s less than $10,000 today-for a life-altering injury. One woman, after losing her uterus, said in court: “I didn’t want to be a statistic. I wanted to be heard.” But the system didn’t listen until it was too late.The Company Knew. They Kept Selling.
Here’s the worst part: A.H. Robins knew the string was dangerous. Internal documents later revealed that by March 1972, the company had clear evidence the string caused infections. Yet they kept selling the device. In fact, they inserted over one million more Dalkon Shields after that point. Doctors were told to keep using it. Clinics were told it was safe. When women started reporting pain and fever, the company blamed poor hygiene or pre-existing conditions. They didn’t recall the product. They didn’t warn doctors. They didn’t stop. Dr. Russell Thompson, who had inserted hundreds of Dalkon Shields, testified before Congress in the mid-70s: “The government wasn’t controlling these kinds of dangerous things that the doctors were putting into women’s bodies.” He wasn’t angry at the women. He was angry at the system that let this happen.
The Law Changed Because Women Suffered
Before the Dalkon Shield, the FDA only regulated drugs. Medical devices? They were treated like kitchen appliances. No testing. No oversight. No accountability. The scandal forced Congress to act. In 1976, the Medical Device Amendments were passed. For the first time, the FDA had the power to require safety and effectiveness data before a device could be sold. They created a classification system: Class I (low risk), Class II (moderate), and Class III (high risk). The Dalkon Shield would have been Class III-and never approved. This wasn’t a minor update. It was a revolution in medical safety. The same rules that now govern your pacemaker, your hip implant, and your modern IUD started because of the Dalkon Shield.The Aftermath: IUDs Vanished for Decades
The fallout wasn’t just legal. It was cultural. After the scandal broke, women stopped trusting IUDs. Doctors stopped offering them. Manufacturers stopped making them. By 1986, virtually no IUDs were available in the U.S. market. The fear wasn’t just about one device-it was about the entire category. It took nearly 20 years for new, safer IUDs to reappear. Today’s devices-like Mirena and Paragard-use single-filament strings that don’t wick bacteria. They’ve undergone years of testing, post-market surveillance, and strict FDA review. They’re safe. But they’re only safe because the Dalkon Shield taught us how not to design them.
Why This Still Matters Today
The Dalkon Shield wasn’t an accident. It was negligence wrapped in corporate greed and regulatory blindness. Today, we still see the same patterns. New reproductive technologies-like at-home fertility monitors, hormone patches, or digital birth control apps-are rushed to market without long-term data. Companies still prioritize speed over safety. Women’s health is still treated as an afterthought. The lesson isn’t just about strings or bacteria. It’s about who gets to decide what’s safe. When women’s bodies are treated as test subjects without consent, when profit outweighs harm, when regulators are asleep at the wheel-people get hurt. The Dalkon Shield is a ghost in the machine of modern healthcare. It’s why we have FDA oversight. Why we demand clinical trials. Why we question every new contraceptive before we trust it. It’s also why we still need to listen to women when they say something hurts.What We Learned
- The Dalkon Shield’s string was a wicking hazard-cotton fibers pulled bacteria into the uterus.
- A.H. Robins ignored internal warnings in 1970 and sold over a million more units after confirming the danger in 1972.
- More than 300,000 lawsuits were filed. Nearly $3 billion in damages were awarded.
- 18 women died. Over 200,000 developed PID. Many lost their fertility.
- The 1976 Medical Device Amendments gave the FDA authority to regulate devices-something that didn’t exist before.
- Modern IUDs use single-filament strings, a direct response to the Dalkon Shield’s design flaw.
- Contraceptive use dropped by over 90% after the scandal, and IUDs didn’t return to the market until the 1990s.
Why was the Dalkon Shield ever approved if it was so dangerous?
The Dalkon Shield was approved under the FDA’s ‘grandfather clause,’ which allowed medical devices to be sold without clinical trials if they were deemed ‘substantially equivalent’ to older models. At the time, the FDA had no authority to test devices for safety-only drugs. The company exploited this loophole, skipping proper testing and rushing the product to market.
How many women were affected by the Dalkon Shield?
Over three million women in the U.S. used the Dalkon Shield between 1971 and 1974. More than 200,000 developed pelvic inflammatory disease, over 100,000 suffered permanent injuries like infertility or hysterectomy, and at least 18 women died. Nearly 300,000 lawsuits were filed, making it one of the largest product liability cases in U.S. history.
Did the company face consequences?
Yes-but not enough. A.H. Robins filed for bankruptcy in 1985 to manage over $3 billion in legal claims. They created a $615 million settlement fund before being bought by American Home Products in 1989. Most victims received only $750 to $2,000 in compensation, while executives avoided criminal charges. The company’s leadership never faced jail time.
Are modern IUDs safe today?
Yes. Modern IUDs like Mirena, Kyleena, and Paragard use single-filament strings that are sealed at both ends, eliminating the wicking effect that made the Dalkon Shield deadly. They undergo rigorous FDA testing before approval and are monitored for safety after release. The regulatory system that protects them today was created because of the Dalkon Shield disaster.
What changed in medical regulation after the scandal?
The 1976 Medical Device Amendments gave the FDA the legal power to require safety and effectiveness data before any medical device could be sold. It created a classification system (Class I, II, III) based on risk. Devices like IUDs, pacemakers, and surgical implants now must go through clinical trials. This was a direct result of the Dalkon Shield scandal.
Why didn’t women speak up sooner?
Many women didn’t realize their pain was linked to the IUD. Doctors dismissed symptoms as unrelated infections or normal side effects. There was also deep stigma around reproductive health-women were often shamed for discussing sexual or gynecological issues. By the time they connected the dots, many were already seriously injured. The legal system then made it worse, forcing victims to relive trauma in court.
The Dalkon Shield didn’t just kill women. It broke trust. It silenced voices. It exposed how little value was placed on women’s lives in the name of profit and progress. But it also gave us the tools to fight back. Today’s safer contraceptives exist because women suffered-and refused to be forgotten.