AI Sexual Health Bias Calculator
How Bias Impacts Sexual Health AI
This tool demonstrates how demographic factors affect AI diagnostic accuracy in sexual health tools. Based on research, AI models show significant accuracy gaps for underrepresented groups.
Sexology isn’t what it used to be. A century ago, it was mostly about pathologizing differences-classifying behaviors as deviant, ignoring women’s needs, and erasing LGBTQ+ identities. Today, it’s being rebuilt by something unexpected: artificial intelligence. But this isn’t just about better diagnostics or faster chatbots. It’s about who gets heard, who gets helped, and who gets left behind when algorithms make decisions about our bodies.
AI Is Changing How We Diagnose Sexual Health
Doctors used to rely on symptoms, lab tests, and experience. Now, AI can scan a pelvic ultrasound and spot signs of endometriosis with 91% accuracy-something human radiologists often miss because the condition looks different in every patient. Algorithms trained on millions of clinical records can now predict STI risk from basic patient data with 89-94% precision, compared to 76-82% for traditional methods. That’s not magic. It’s data.
But here’s the catch: most of that data comes from cisgender men. Studies show AI models trained on these skewed datasets are 15-30% less accurate for women, trans people, and nonbinary individuals. One fertility app, built using data from cis women, told a trans man he was ovulating when he wasn’t-delaying his transition care by months. That’s not a glitch. It’s a design flaw.
AI can also analyze dental X-rays and bone scans to determine biological sex with over 90% accuracy. That sounds useful for forensic work or unclear medical cases. But what happens when that same tech is used in clinics to guess someone’s gender based on anatomy? It forces people into boxes that don’t fit. And in places where being trans is criminalized, that kind of tech doesn’t help-it endangers.
The Chatbots That Talk Back
For years, sexual health education felt like a lecture from a textbook. Now, chatbots like Amanda Selfie-designed with a Black transgender woman avatar-are reaching people who never walked into a clinic. In pilot programs, these bots saw 37% higher engagement than traditional health portals. Why? Because users didn’t feel judged. They didn’t have to explain their identity. They just asked.
Teens, especially, prefer talking to an AI. A Planned Parenthood study found 82% of adolescents felt more comfortable asking about contraception, STIs, or identity through a bot than a nurse. But here’s where it breaks: 43% of those same teens got frustrated when the bot couldn’t understand terms like “nonbinary,” “hormone therapy,” or “top surgery.” One user asked, “Can I get pregnant if I’m on testosterone?” and got a canned answer about ovulation cycles. The bot didn’t know the question was valid.
And then there’s misinformation. A Johns Hopkins audit found 68% of AI tools gave conflicting advice about emergency contraception. Some said it works up to 72 hours. Others said 120. One even claimed it causes infertility. These aren’t small errors. They’re life-altering.
Who Built This? And Who’s Missing?
Right now, 89% of AI sexual health tools come from North America and Europe. Yet 76% of the world’s sexual health burdens-STIs, unsafe abortions, lack of access to care-are in low- and middle-income countries. That’s not a coincidence. It’s a power imbalance.
Most startups chasing this market have teams of engineers and marketers. Very few have sexologists, community health workers, or people from the communities they’re trying to serve. Crunchbase data shows only 22% of these companies have dedicated teams working on equity. That means algorithms are built by people who’ve never had to choose between rent and an STI test. They don’t know what it means to code-switch just to get accurate info.
And the data? It’s worse than biased-it’s invisible. Trans people, intersex individuals, people of color, disabled folks-they’re not just underrepresented in training sets. They’re often excluded entirely. One study found 79% of mainstream AI tools didn’t recognize gender-affirming care terminology. If you type “hysterectomy after transition,” the system doesn’t understand. It just gives you a generic answer about reproductive health.
Regulation Is Catching Up-Slowly
In January 2025, the FDA said any AI tool claiming to diagnose STIs, infertility, or hormonal conditions needs 510(k) clearance. That’s a big deal. It means 63 existing apps now have to prove they’re safe and accurate. But clearance doesn’t mean ethical. It just means they passed a technical bar.
The WHO released ethical guidelines in March 2024 that demand three things: (1) at least 30% of training data must come from underrepresented groups, (2) every AI tool needs a third-party bias audit, and (3) users must be told when they’re talking to an algorithm. Simple rules. Hard to enforce.
And then there’s the legal mess. In the U.S., 47 states have different laws about how AI can handle reproductive health data. In one state, an app can share your search history with law enforcement. In another, it’s illegal. That means a tool that works in California might be banned in Texas-even if it saves lives.
The Human Cost of Automation
AI doesn’t feel shame. It doesn’t cry when a patient says, “I’m scared to tell my family I’m queer.” It doesn’t pause when someone says, “I was raped.” No algorithm can replace a clinician who knows when to listen, when to hold silence, and when to say, “Let’s get you help.”
Studies show AI accuracy drops to 68% for complex cases like sexual dysfunction, chronic pain, or trauma-related intimacy issues. Human specialists? 89%. That gap isn’t about technology. It’s about empathy. And that’s something no model can learn from data alone.
There’s also the risk of surveillance. One NIH study found fertility apps were selling user data to third parties-data that could be used to deny someone reproductive rights in states with abortion bans. Imagine being tracked because you searched for “period delay pill” or “transgender hormone therapy.” That’s not healthcare. That’s control.
What’s Next? The Fight for Ethical AI
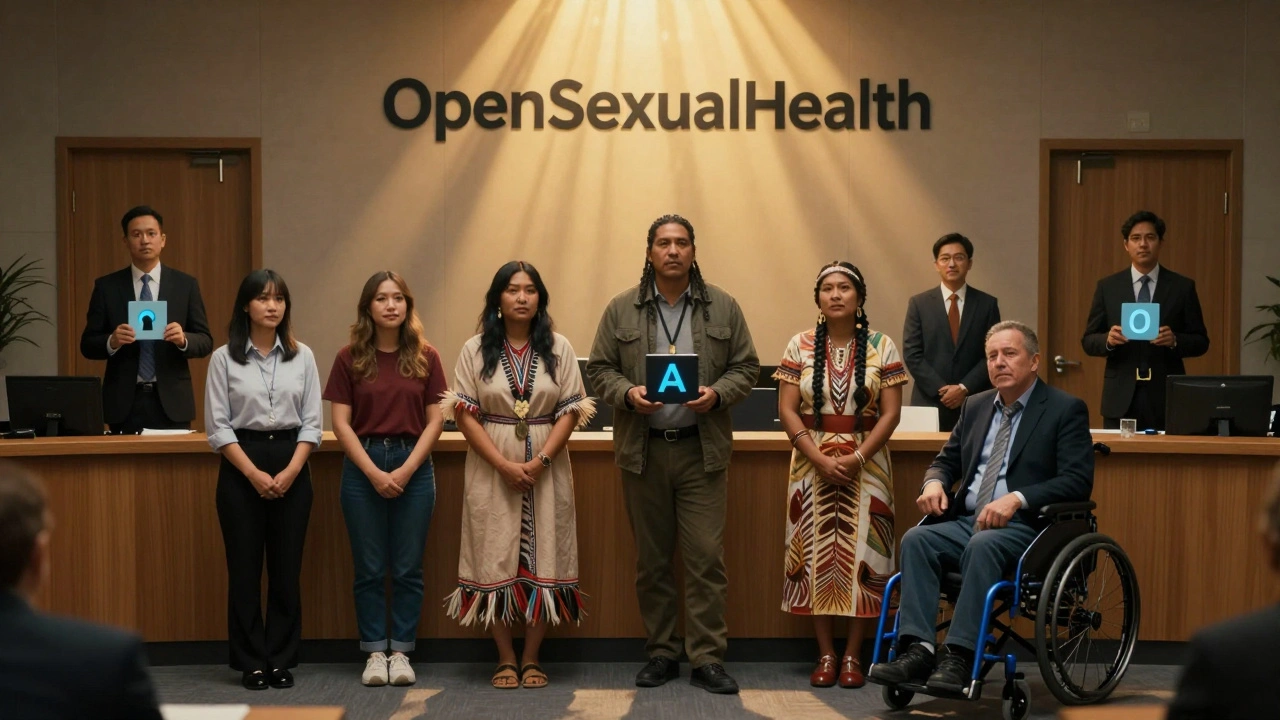
The NIH just launched a $45 million initiative called “AI for Equitable Sexual Health.” That’s a start. But money alone won’t fix this. We need people-real people-on the teams building these tools. We need trans sexologists, Black nurses, Indigenous healers, disabled advocates. We need them in the room when the code is written.
Open-source projects like OpenSexualHealth are showing it’s possible. Their tools are 95% transparent-every line of code, every dataset, every bias test is public. Compare that to proprietary tools, where only 62% of documentation is complete. Transparency isn’t optional. It’s survival.
The future of sexology won’t be decided by tech companies. It’ll be decided by who gets to speak, who gets to be seen, and who gets to say no.
AI can help us diagnose faster, reach farther, and break down stigma. But if we let profit drive design, if we ignore history, if we let bias go unchecked-then we’re not advancing sexology. We’re automating oppression.
The real question isn’t whether AI will change sexology. It’s whether we’ll change AI before it changes us.




